10 healthcare technology trends for 2025
Des 17, 2024 - Reading time 8-10 minutes
Faced with ongoing staff shortages and growing patient demand, healthcare organizations around the world are being compelled to rethink how and where they deliver care. There is also a growing recognition of the importance of reducing the sector’s environmental impact. These 10 healthcare technology trends highlight the potential of innovation to help deliver better care to more people, in a sustainable way.

1. Generative AI: a time-saving virtual assistant
With staff stretched thin, healthcare leaders are turning to automation to reduce the burden on healthcare professionals. The 2024 Philips Future Health Index report showed that 92% of surveyed healthcare leaders think automation is critical for addressing staff shortages by relieving them of repetitive tasks and processes. An equal percentage believe it will save healthcare professionals time by reducing administrative work, allowing them to spend more time with patients.
Generative AI has emerged as a powerful tool supporting this healthcare technology trend, promising to boost clinician productivity in ways that seemed impossible just a few years ago. It’s no wonder that 85% of healthcare leaders worldwide are already investing or plan to invest in generative AI within the next three years. We expect this trend to accelerate in 2025 as the sector continues to explore ways of gaining workflow efficiencies with generative AI.
Already today, generative AI can function as a virtual assistant to save healthcare professionals valuable time, using large language models to organize clinical notes and simplify the ways patient information is communicated across teams. In areas like cancer care, generative AI could be a game-changer by summarizing vast historical reports to give care teams immediate insights into a patient’s history. It could also speed up reporting and translate complex medical information into common terms, helping to engage patients more in their own care.

2. Simplifying complex diagnostics with AI
While AI can significantly streamline administrative tasks and improve patient engagement, its role in healthcare extends beyond automation. AI can also elevate the skills of healthcare professionals. With experienced staff in short supply in many healthcare systems around the world, AI can help simplify complex diagnostics, enabling less experienced professionals to provide high-quality care with confidence.
For example, recent advances in AI have made cardiac CT easier to use, making it accessible to more facilities to increase capacity and deliver better cardiac care to more people. In addition, less experienced technicians can rely on remote consultations and expert training for virtual support and reassurance. Similarly, embedding AI in ultrasound systems allows physicians to detect, diagnose and monitor cardiac conditions more confidently and efficiently.
Integrating AI into cancer treatments can also enhance patient care by addressing the increased risk of heart disease associated with therapies such as radiation and chemotherapy. Studies show that adult cancer survivors across a wide range of cancers face a 37% higher risk of developing cardiovascular disease [1]. The latest AI technologies can quickly detect signs of cardiotoxicity early in the treatment process by automating and accelerating echocardiographic measurements. Improved reproducibility and shorter study times make the process more efficient and reliable, reducing the risk of treatment delays. That’s good news for cancer patients who may otherwise face serious heart issues alongside their recovery.

3. A silent revolution in surgery
A silent revolution in surgery is marching ahead as minimally invasive procedures continue to replace traditional open surgeries. These minimally invasive procedures are transforming how providers treat cardiovascular conditions, offering patients faster recovery, reduced pain and fewer complications.
With the introduction of new technologies in interventional care, minimally invasive procedures have become more advanced – but also increasingly complex. Physicians need to collect and analyze data from a wide range of sources, such as live 2D X-ray images, 3D ultrasound, Intravascular Ultrasound (IVUS), and FFR or iFR physiological flow measurements, all while closely monitoring the patient. That’s why integration of systems, software and devices has become increasingly important. This integration allows interventional physicians to treat patients with greater control and confidence during every stage of minimally invasive cardiac procedures.
The latest innovations in image-guided therapy also offer a unique opportunity to expand access to life-saving stroke care. Every two seconds, someone on Earth has a stroke, making it the second leading cause of death and a major cause of long-term disability. Yet less than 5% of our global population has access to mechanical thrombectomy, a minimally invasive treatment that has shown to be highly effective [2]. Expanding access by increasing the number of stroke-ready hospitals and training healthcare professionals in the latest interventional techniques is a cause that Philips is committed to, in partnership with the World Stroke Organization.

4. Seeing the full patient picture in critical care
In critical care, time is crucial – yet always in short supply. Healthcare professionals often lose valuable time pulling patient data together from disparate sources. An open ecosystem approach to patient monitoring can help overcome this challenge by allowing data to flow freely across healthcare technology from different vendors. This creates a unified, standardized patient view that is accessible from anywhere in the hospital.
In 2025, expect further advances in patient monitoring based on this open ecosystem approach to healthcare technology. Medical device integration and vendor-neutral interoperability in critical care are already helping healthcare organizations improve clinical efficiency and data accuracy, while freeing up staff to focus on providing patient-centered care. Advancing common interoperability standards with industry partners will further enhance this approach, giving systems and devices a common language to ‘speak to each other’ so that patient information can be shared even more easily.
By breaking down data silos, we will also see further development of algorithms that can help care providers predict and prevent adverse patient events. We are just beginning to explore the potential of advanced analytics in critical care, using smart rules to provide care teams with actionable alerts for emerging events. In the future, AI will offer increasingly personalized recommendations by comparing the full patient picture with thousands of similar cases to help determine the best approach for each patient.

5. The home is the new hospital room
While the previous four healthcare technology trends all focus on improving hospital care, there is an equally important trend that will continue to gain traction in 2025: the ongoing shift to managing health outside of the hospital. Hospital-at-home programs for patients who need acute-level care continue to be on the rise, allowing patients to receive high standards of care wherever they are, not just in hospital settings.
Remote patient monitoring plays a critical role in this shift by providing healthcare professionals with real-time data to manage patient care from a distance. It has also been shown to be effective in reducing hospital readmissions for patients with chronic diseases such as congestive heart failure and is increasingly used in post-operative monitoring for early and safe patient discharge. Hospitals get to free up scarce beds for patients who need them more urgently, while patients benefit from an improved experience at home.
In 2025, we will see further advances in AI and predictive analytics to support remote detection of patient health risks based on vital signs and other data. In fact, our 2024 Future Health Index report shows that remote patient monitoring is the biggest area of planned AI implementation over the next three years, with 41% of healthcare leaders intending to invest in it. This will not only help prevent complications and hospitalizations by enabling timely interventions, but also improve quality of life for patients, offering them peace of mind as they receive care in their own homes.

6. Telehealth reaches patients where they are
The use of virtual care soared during the COVID-19 pandemic. Today, it offers an opportunity to change how healthcare is delivered around the world by improving healthcare outcomes, particularly in resource-limited settings. Bringing care directly to patients in medically underserved communities or regions is an essential part of improving access, equity and affordability of patient care.
From remote patient monitoring and point-of-care ultrasound to real-time video consultations and more, telehealth increases the potential for healthcare to reach more people, no matter where they’re located. It can also reduce the need for specialist visits, as primary care physicians can resolve 40% of issues with the help of telehealth-based specialists [3].
For example, telemedicine capabilities allow sonographers and patients based at satellite locations to connect virtually with doctors to discuss ultrasound findings in real time. These more remote locations have every capability of the main practice – without either party needing to drive several hours. Similarly, digitalization, informatics and AI are improving the quality and accessibility of obstetric care in low-income countries and underserved communities. Interpretation of images obtained through AI-enabled handheld ultrasound is no longer required by the operator, which reduces the training needed to perform the exam.
Telemedicine is now being embraced around the world. For instance, healthcare providers in Indonesia – which faces unique accessibility challenges as the world’s largest country comprised solely of islands – are embracing digital health transformation to improve healthcare accessibility and quality, in line with the government’s healthcare strategy. Telemedicine, remote patient monitoring and AI are among the tools that the country will use to provide patients with care, even in remote areas.

7. Data and digital health are driving tech-savvy parenting
Modern parenting has taken on a decidedly digital flavor with the integration of smart devices and apps into childcare routines. Parents now have unprecedented access to data that can help them make informed decisions and receive reassurance about their child’s overall health and well-being. In fact, there’s growing interest in AI-enabled technologies that not only provide monitoring capabilities but also deliver predictive insights about a child’s behavioral patterns.
As we move into 2025, we expect an increasing number of parents – particularly first-time parents – to embrace apps and connected devices to help keep a watchful eye on their children. Our research has shown that 80% of parents in the US and 79% of parents in Europe are open to using wearables and smart technologies [4,5], demonstrating the growing desire to implement care routines based on data to support their children’s safety and health.
Households are becoming more connected through the adoption of smart home systems, allowing parents to conveniently access device features such as video and audio feeds on their phones or computers. Wearables and smart devices like socks, pacifiers and trackers can provide real-time information about a child’s activities or vital signs, including respiratory patterns, body temperature and heart rate. Some AI-enabled baby monitors can help caregivers decode an infant’s cries, allowing for quicker responses to hunger and other needs.
It's clear that digital health tools are transforming modern parenting in remarkable ways. And while these smart technologies aren’t a replacement for active, hands-on caregiving, these devices can offer actionable information, while also giving parents peace of mind.

8. Innovating for sustainability – with sustainable AI
As highlighted in several of the healthcare technology trends above, AI holds immense potential to transform healthcare, increase efficiency and improve lives. And now, AI is also starting to help improve sustainability for companies – including within healthcare technology.
Healthcare accounts for 4.4% of global CO2 emissions [6] – more than either the aviation or shipping industries. AI could help analyze supply chains and identify areas for improvement, reduce waste, or improve facility management. Operational efficiencies like this are just the start. AI is also already helping to increase imaging speed, translating into lower power consumption per patient scan. How AI can be leveraged to reduce global healthcare emissions and environmental impact is an area ripe with potential for 2025 and beyond.
But along with widespread adoption comes the potential for unintended consequences and significant environmental impact. There’s growing awareness of the need for sustainable innovations and AI models. Healthcare systems are now questioning how AI may be adding to their carbon footprints, while developers are concerned about improving the sustainability of the models.
Why? Because digital solutions need significant energy and materials to generate, process and store data, along with water to cool heat-intensive data centers – all contributing to healthcare’s carbon footprint. In fact, the energy consumption of AI is increasing annually between 26% and 36%, and the power usage of data centers could triple within four years [7]. E-waste is another major issue to consider. Generative AI is also expected to generate up to 2.5 million tons of e-waste by 2030 [8]. As we digitalize healthcare, companies are recognizing that managing and minimizing the energy, material and water needs for AI will be essential to ensure the least impact on the environment.

9. Collaboration to reduce supply chain emissions
The vast majority of healthcare’s carbon footprint – 71% – comes from supply chains through the production, transport and disposal of goods and services [9]. In fact, reducing these Scope 3 emissions is expected to have seven times more impact than just lowering a company’s own emissions. Healthcare organizations are increasingly recognizing the importance of addressing supply chain emissions not just for upcoming government regulations and reducing overall environmental impact, but also for their own financial performance. They are teaming up with partners throughout their value chains to drive change.
Greater transparency and sustainable decision-making are already becoming major considerations in supply chains, from circular product design to collaborations with suppliers. According to the 2024 Future Health Index report, over the next three years, 41% of healthcare leaders plan to choose suppliers with sustainable targets and initiatives, and an equal percentage plan to implement sustainable procurement strategies, including circular equipment. Some companies like Philips are working directly with their suppliers to ensure they meet environmental standards and adopt sustainable practices. This type of responsible sourcing of goods and services can have a positive ripple effect within the entire healthcare value chain.
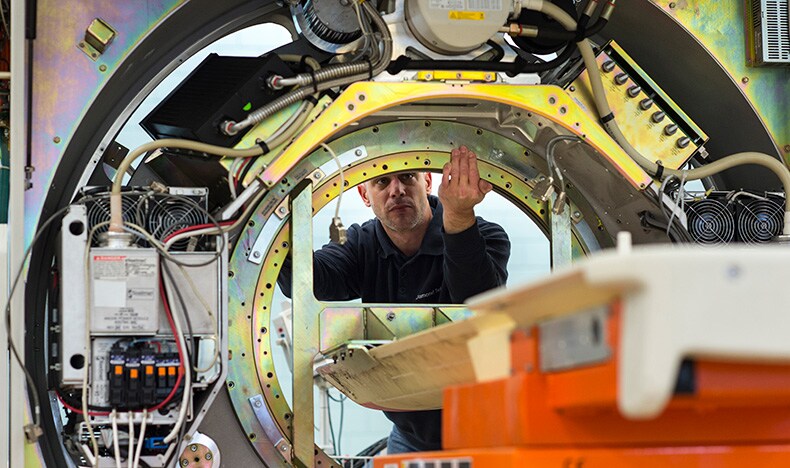
Meanwhile, adopting circular practices, which emphasize using less, using longer, and using again, is another way that both healthcare organizations and their suppliers are significantly reducing raw material usage and waste. Refurbishment is one example. Both refurbished consumer products and refurbished medical devices, including image-guided therapy systems and MRI scanners, offer sustainable and cost-efficient alternatives without compromising performance. The refurbished medical devices market is expected to grow from $17.05 billion in 2024 to $30.78 billion by 2029 [10]. By embracing collaborative efforts, healthcare organizations can significantly reduce their environmental impact.
10. Building resilient healthcare systems with technology to adapt to climate change
As climate change poses increasingly significant challenges, there is an urgent need for hospitals and healthcare systems to enhance their preparedness. The World Health Organization reports that climate change is already impacting health in many ways, including death and illnesses from heat waves, drought, floods, air pollution, wildfires and more [11]. Many healthcare facilities see increasing numbers of patients with climate-related health issues, yet not all are prepared to care for the influx. Issues extend beyond patient care – healthcare must also consider the impact on their own operations and facilities.
In 2025, as the global conversation turns toward this topic, we expect that healthcare technology will play an important role in ensuring that the healthcare industry is equipped to handle these growing challenges. One way is through developing resilient infrastructure to ensure continuous and effective healthcare delivery, even in the face of climate disasters. This includes transitioning healthcare facilities to renewable energy sources and implementing sustainable practices to reduce their carbon footprint and operational costs.
There are also opportunities for increased training and education programs to equip healthcare providers with the knowledge and skills needed to manage the influx of heat-related illnesses and vector-borne diseases. Additionally, early warning systems could enable prompt responses to minimize health risks, and strengthening community health programs can help improve preventive care and manage climate-sensitive health conditions at the local level.
By embracing such initiatives, the healthcare industry can better adapt to the impacts of climate change and ensure a healthier future for all.

Sources [1] https://www.jacc.org/doi/10.1016/j.jacc.2022.04.042 [2] https://www.ncbi.nlm.nih.gov/books/NBK562154/ [3] https://hbr.org/2022/05/the-telehealth-era-is-just-beginning [4] Philips Pregnancy+ user survey, 2022 [5] Philips Pregnancy+ parents survey conducted by InSights Consulting, November 2022 [6] https://noharm-global.org/documents/health-care-climate-footprint-report [8] https://www.nature.com/articles/s43588-024-00712-6 [9] https://noharm-global.org/documents/health-care-climate-footprint-report [11] https://www.who.int/news/item/02-11-2023-climate-change-and-noncommunicable-diseases-connections





